Complete guide to AI Powered VR Education
Why 2025 Is the Year of AI-Powered VR
The nursing shortage is here — and it’s urgent. In 2022 alone, more than 76,000 qualified students were turned away from U.S. baccalaureate nursing programs, primarily due to a lack of clinical placements and limited faculty capacity (AACN, 2022).
At the same time, educators are expected to prepare more nurses, faster, while ensuring graduates are confident, competent, and practice-ready. Traditional labs and clinical placements simply cannot scale to meet demand. Student anxiety around NCLEX pass rates only adds to the pressure.
“This is a global problem. Every university is facing it, and every year we look for new ways to improve education methods despite resource pressures.” — Winston-Salem State University
That’s why AI-powered virtual reality (VR) is gaining momentum in 2025. Unlike mannequins or screen-based simulations, AI-powered VR creates emotionally responsive virtual patients, adaptive feedback loops, and repeatable high-stakes scenarios. Students get real-life training without real-life risk, and educators gain a scalable tool to boost competence, confidence, and outcomes.
“AI-powered VR allows students to face patients who respond like humans, practice decision-making under pressure, and repeat until mastery. This is the next frontier of nurse education.” — Dr. Tori Brown
Importantly, 2025 also marks the year when VR met the challenge of mental health education. Previous VR simulations struggled to replicate the complexity of psychiatric care. New AI-powered platforms, however, now provide realistic, adaptive mental health simulationsNow, technology has solved the problem, but not all services offer the same level of high quality AI powered simulations to do this well.
What Is AI-Powered VR in Nursing Education?
VR itself isn’t new — it has long been used in gaming and early healthcare training. What’s new is the AI integration that makes VR simulations dynamic, adaptive, and human-like.
With Patient Ready’s AI-powered VR:
Students face patients who express emotions like pain, confusion, or gratitude.
The system adapts in real time to their decisions.
Educators can measure both hard skills and soft skills such as empathy, communication, and clinical judgment.
This mirrors real-world nursing: not just procedures, but judgment, prioritization, communication and empathy under pressure.
Why It Matters: Evidence From Research
1. Barriers to Clinical Placements
Nursing schools are struggling to keep up with patient demand. The #1 reason qualified applicants are turned away is lack of clinical placements (AACN, 2022). VR directly addresses this bottleneck by offering scalable, safe practice inside the classroom.
2. Clinical Judgment & NCLEX Alignment
AI-powered VR scenarios can be mapped directly to the Next-Gen NCLEX Clinical Judgment Measurement Model (NCLEX, 2023), giving students practice in recognizing cues, prioritizing interventions, and taking action.
3. Knowledge, Skills, Retention & Satisfaction
A 2023 meta-analysis of 12 randomized controlled trials (1,167 students) found VR significantly improved theoretical knowledge, skills, retention, and satisfaction compared to traditional methods (BMC Medical Education, 2023).
70% of BSN students believe AI should be incorporated into nursing education to improve confidence and learning (University of Texas, Austin).
Research from the University of Texas Rio Grande Valley (2025) found statistically significant improvement in student performance pre- and post-test using AI-powered VR simulations.
A 2024 systematic review confirmed VR reduces time to perform skills while boosting confidence and satisfaction (MDPI, 2024).
4. Improved Student Performance
At Winston-Salem State University, VR implementation led to a 7-point increase in average exam scores. Nearly every student agreed VR was valuable for applying theory to practice (Brown et al., 2023).
5. Safety & Risk Reduction
VR offers a safe space to fail. A 2023 study found new interns trained in VR had fewer needlestick injuries and higher confidence than those without VR training (PMC, 2023).
“The fact I can make a mistake and try again reduces my anxiety.” — Student, Queens University using Patient Ready
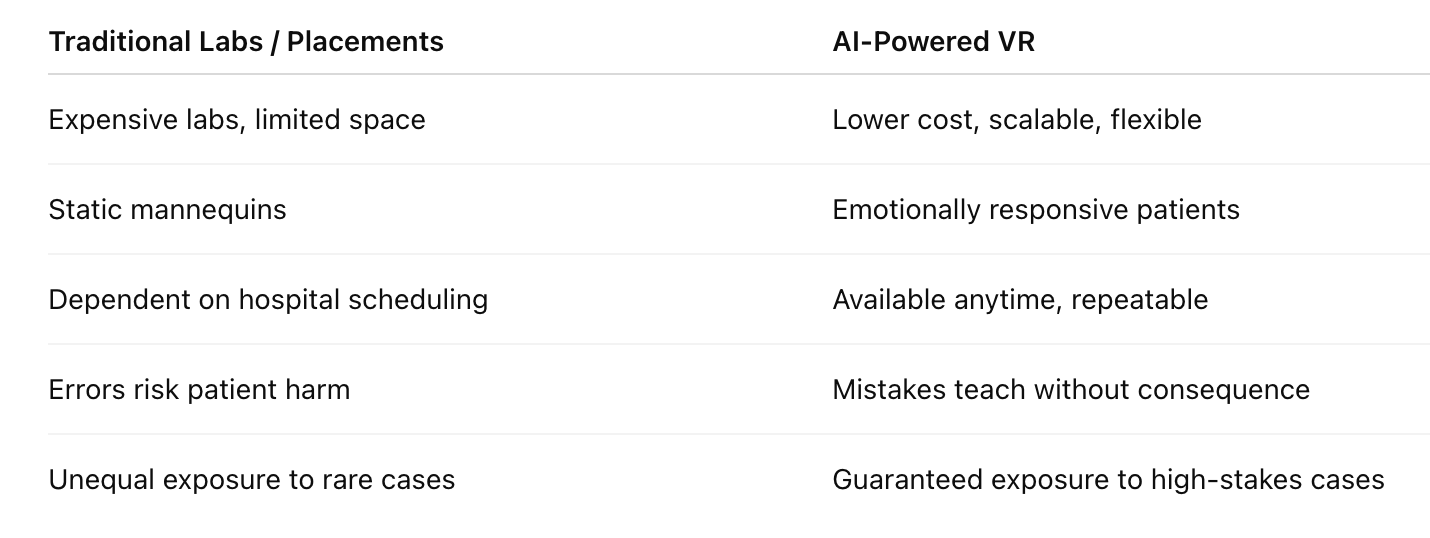
VR vs. Traditional Simulation: The Clear Difference
Traditional education and AI powered VR comparison table
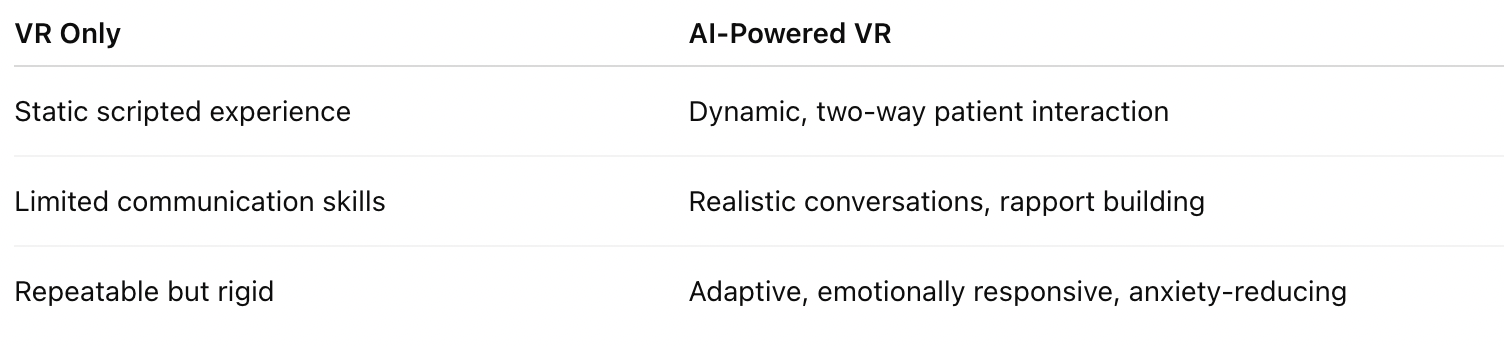
VR vs. AI-Powered VR - Not all VR is created equal.
VR and AI-powered VR comparison table
With Patient Ready, educators don’t need to “upgrade” old VR — our platform was built with AI at the core, designed to simulate the full complexity of clinical environments. From angry parents to hesitant patients, learners face characters who feel, respond, and react just like real humans
ROI: Why It Pays Off for Programs
Up to 50% of clinical hours can be replaced with high-quality simulation while maintaining NCLEX outcomes (NCSBN).
Cost savings: VR can cut costs by as much as 40% while boosting scores 5–6% (Nightingale College, 2023).
Faculty efficiency: One educator can oversee multiple students simultaneously.
Pass rates: Programs that integrated VR during clinical shortages maintained or exceeded NCLEX pass rates (Clinical Simulation in Nursing, 2025).
The Future: Why Patient Ready Leads
The VR healthcare market is set to grow exponentially, but technology alone isn’t enough. Patient Ready is designed for nurse educators who demand more than flashy tools:
Emotionally responsive patients > real empathy training
Safe, repeatable practice > competence through mastery
Proven results > higher exam scores and NCLEX pass rates
Though new to the market (3 years), Patient Ready pioneered AI for nurse education and can help programs integrate within 90 days — with hands-on support every step of the way.
How to Integrate AI-Powered VR in 90 Days
Set Up – Establish requirements, integration roadmap, and curriculum fit.
Faculty Training – Ensure comfort with VR use and performance dashboards.
Curriculum Mapping & Grading – Align simulations to NCLEX, create grading rubrics, track outcomes via dashboards.
Implement – Start small, gather outcome data, expand strategically.
Scale & Refine – Adjust scenarios, measure performance, and expand program-wide.
Book a Demo with us Now for two-months free access
Transform your curriculum with hands on support from the team at Patient Ready. We’re Ready to go!
FAQs
Q: Can VR replace clinical hours?
Yes. The NCSBN found up to 50% of clinical hours can be replaced with high-quality simulation without negative effects on outcomes (Hayden et al., 2014).
Q: Does VR improve NCLEX readiness?
Yes. VR scenarios can be designed around the NCLEX Clinical Judgment Model, strengthening decision-making.
Q: How quickly can VR be implemented?
Most programs can launch within 90 days, from training to curriculum mapping.
Q: What is the ROI?
VR can reduce costs by up to 40% while boosting scores and pass rates.
References
AACN (2022). Nursing schools see enrollment increases but turn away 76,140 qualified applicants.
Brown, T. et al. (2023). Reimagining nursing education through virtual reality. Teaching and Learning in Nursing.
Chen, F. Q. et al. (2020). Effectiveness of VR in nursing education: Meta-analysis. JMIR.
Hayden, J. et al. (2014). NCSBN National Simulation Study.
BMC Medical Education (2023). Virtual reality vs traditional teaching: Meta-analysis.
MDPI (2024). VR in healthcare education: Systematic review.
Clinical Simulation in Nursing (2025). Integration of virtual simulation to maintain NCLEX outcomes.
Forbes (2022). AR/VR healthcare market poised to hit $10B.
PMC (2023). VR training reduces needlestick injuries in interns.
Patient Ready AI powered VR